My recollections of sitting my RACGP OSCE (Fellowship clinical exam) are rather hazy, and not just because it was over a decade ago. I do have one bit of advice though – a do-as-I-say-not-do-as-I-did tip – try to avoid traumatic brain injuries in the month leading up to your clinical exam.
Here’s the story of how I came to be doing my RACGP OSCE exams with 6 facial fractures and left temporal lobe contusions….
Saturday, 4th October, 2003.
I couldn’t close my mouth. That wasn’t a good sign. Many a time I’ve been admonished for having my mouth open more than it’s shut, but on this occasion it had nothing to do with being garrulous. My upper and lower jaw no longer occluded. I sat up – gingerly, to discover that I was completely alone in unfamiliar bushland, with no recollection of how I got there. I lay back down and closed my eyes, inappropriately unperturbed.
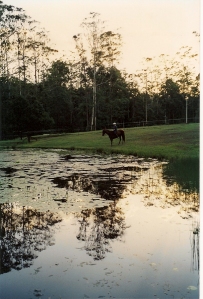
Like a slowly developing Polaroid picture, the details appeared in my mind’s eye. The colours were increasingly vibrant yet the focus remained blurry. I remembered studying for my OSCE exams that morning before deciding to take one of horses for a ride in the State forest to clear my head. The rest was a blank; my head had been cleared too well.
 It was time to play CSI. The skid marks and saddle imprint in the mud clearly showed where Rondo had shied and fallen (probably on seeing a kangaroo – he was terrified of them), and my face had left a lovely impression at its point of impact. Thankfully, Rondo appeared on cue when called – mud-splattered and jittery but unharmed. It took us several hours to find our way out through the maze of interconnected forest trails, what with my disorientation and his being one of those rare horses with no inclination to make a beeline for home. Unlike many males I’ve known, he was excellent at taking direction but hopeless at finding it.
It was time to play CSI. The skid marks and saddle imprint in the mud clearly showed where Rondo had shied and fallen (probably on seeing a kangaroo – he was terrified of them), and my face had left a lovely impression at its point of impact. Thankfully, Rondo appeared on cue when called – mud-splattered and jittery but unharmed. It took us several hours to find our way out through the maze of interconnected forest trails, what with my disorientation and his being one of those rare horses with no inclination to make a beeline for home. Unlike many males I’ve known, he was excellent at taking direction but hopeless at finding it.
I remember only one thing clearly about that long ride home: laughter. My laughter – laughter which bubbled up from deep inside, slipping between my maloccluded teeth and spilling out of my bruised mouth. In my concussive haze my situation somehow seemed side-splittingly humorous. The funny side was the only side I could see.
I laughed more in that next month than I’d done in the preceding three years. Although my personal predicament lost its comedic edge fairly quickly (temporal lobe contusions and six facial fractures requiring two maxillofacial surgeries and a six-week liquid diet do tend to be dampeners), the world around me tickled my funny bone in completely new and outrageous ways. I laughed at the news. I laughed when I got stuck in traffic. I laughed over spilt milk. And most surprising of all, I laughed at corny American sitcoms. You know the ones: weak, predictable story lines, groan-worthy one-liners and canned audience laughter. I found them not only funny, but hilarious. I’d laugh so hard that I’d double up on the floor in stitches with tears streaming down my cheeks. I kid you not.
Despite my looming exams, my neurologist prescribed “brain rest” and instructed me not to study. Nothing I read seemed to be retained anyway, so I put my books aside and indulged in my new-found penchant for mindless entertainment. I laughed the days away without a care in the world.
 Three weeks after my accident, less than a fortnight after two reconstructive surgeries, and against medical advice, I sat my OSCE exam. In my brain damaged state, I was not at all worried about whether I’d pass or fail, happy to turn up and just “have a go”. I don’t remember much of it, other than wondering why my fellow candidates all looked so worried, receiving stern glances from an exam supervisor as I giggled to myself in a rest station, and having to ask one of the role players about her presenting complaint at least three times (my brain simply refused to retain the information).
Three weeks after my accident, less than a fortnight after two reconstructive surgeries, and against medical advice, I sat my OSCE exam. In my brain damaged state, I was not at all worried about whether I’d pass or fail, happy to turn up and just “have a go”. I don’t remember much of it, other than wondering why my fellow candidates all looked so worried, receiving stern glances from an exam supervisor as I giggled to myself in a rest station, and having to ask one of the role players about her presenting complaint at least three times (my brain simply refused to retain the information).
I miraculously passed (although it was far from an outstanding performance!). Somewhat unfortunately, over the following weeks my ability to laugh outrageously at the banal also passed, and my sense of humour crept back to the dry and satirical side of the fence. The news of the world was again depressing, traffic congestion got my goat and split milk, although not inducing tears, no longer triggered a giggle.
I’m not sure if my laughter was the illness or the medicine, but it was definitely an integral part of the healing process. Having a traumatic brain injury was for me a far from unpleasant experience. In fact, it seemed to suggest that life is not only more painless for the brainless, but it is also much funnier.
While sitting a major exam in such a state was entirely without stress at the time, I do not recommend it as a technique to reduce performance anxiety. In all seriousness, I was very lucky to have passed, and believe that the only reason I did was that I had spent the previous 18 months preparing. Not by going home and studying every night, but by engaging in deliberate practice each and every day when seeing patients. Good communication skills and examination techniques were so ingrained that they did not require the concentration and higher level thinking that the knock on my head had temporarily disabled. These semi-automated skills alone are not enough to be a safe and competent doctor in the real world of course, but, together with a big helping of luck, were enough to carry me through the OSCE exam on the day, as I smiled and laughed my way through the stations, completely unfazed.













